Doctors, EMS workers, Psychiatrists share Coronavirus stories
Doctors, EMS workers, Psychiatrists share Coronavirus stories.
While some families are grappling with how to keep their children educated and entertained in this new age of social distancing, many on the front lines are grappling with whether to risk going home to their families some nights or pondering whether responding to an emergency could result in exposure.
The risks and pressures squeezing those on the front lines transcend the health care industry, as essential services are provided by emergency responders, police officers, nurses, doctors, lab clinicians, maintenance workers, administrators, those in transportation, utilities, cleaning and food services and many other interconnected duties that make all lifesaving operations work.
‘Am I going to get exposed on this call?’
“It’s a very strange time. I’ve been in EMS for 25 years. The only other time things were so unknown was when Sept. 11 happened. We have to think twice about every move we make. We have daily, sometimes hourly, reminders about protection.
“We’ve always talked about pandemic planning in the past; this is the first time we’ve ever been in a live event. As a paramedic and EMT, we are used to dealing with emergencies snowstorms, fires, accidents but with this type of disaster, there is no forecasted end to it.
“There is a heightened sense of anxiety as we encounter patients in the field who are symptomatic. With the news coming in of younger patients with signs of respiratory failure needing hospitalization, the question as we go out is: ’Am I going to get exposed on this call?’
“It’s not a matter of if we are going to get exposed; it’s when. How many and what will be the loss for EMT and paramedic staffing? We already have staffing problems to begin with, and this will make it worse.
“… I’ve encountered one suspected case so far. I felt confident in the training and protection equipment I had that I was protected. We are not tested until we show signs and symptoms of the virus.
“A lot of EMS services have financial concerns. We are seeing a drastic reduction in 911 calls. We rely on providing services, and like other businesses, the sharp reduction in calls will mean a sharp reduction in revenue and will be a concern for a lot of EMS agencies.”
Chief Evan Resnikoff, president of the Bucks County EMS Chiefs Association and chief of Newtown EMS
‘What a time to deal with bureaucracy’
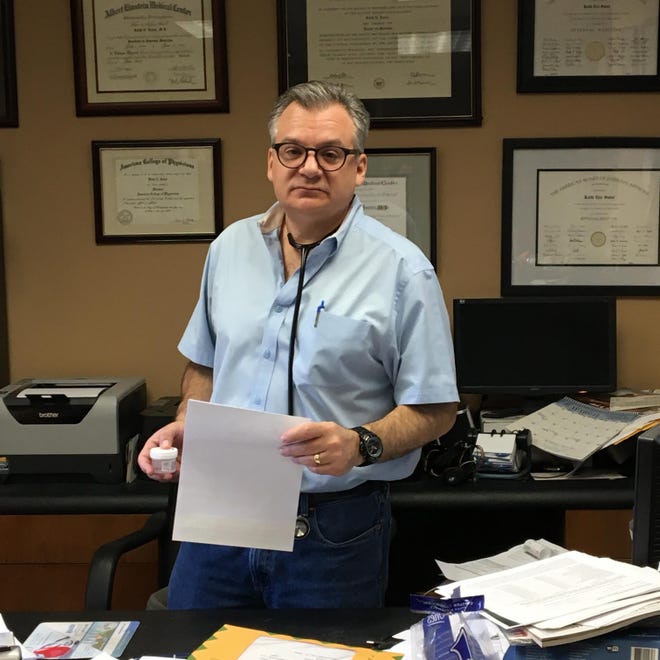
“We are a teeny, tiny office with a small, very supportive ancillary team.
“We are learning and teaching right on the job, implementing ’telehealth’ with seniors, some who are not so savvy with a smartphone even.
“We are asking them to sign on, access a computer screen, tell us their problems … all while remaining calm.
“… There are multiple frustrations but multiple signs of humanity.
“Filtering through calls of real medical need. Filtering through calls of acting as therapist. Filtering through calls for a long to-do list.
“We are running a practice on short staff. As one person gets sick, another doubles up in duty. But we are doing it.
“But we are people, too … and while we are calming everyone, we also have our own nerves to quell, late in the night … most usually at 3 a.m.
“We have financial burdens as well.
“Will this great new frontier called telehealth get paid?
“Each of the insurances (and there are plenty) … have different rules and different guidelines and different caveats. … So while we are on the front line … we have to worry about the rule book. What a time to deal with bureaucracy.
“There are those asking for malaria drug prescriptions and those who just want to have a human voice on the other line.
“There are those who call and tell us the COVID testing swab wasn’t done properly and those that are impatient with results.
“Some specialists are closed and patients need their meds … so we end up with patients calling us when there is no one else to talk to.”
Vivi Sadel, administrator with Keith Sadel Internal Medicine, Southampton
Running on all cylinders
This is according to Dr. Gerard Cleary, chief medical officer at Abington Hospital-Jefferson Health:
It was raining Monday afternoon, and the steady downpour had soaked security personnel at Abington-Jefferson Health, where a line of drivers snaked around a hospital parking lot to access coronavirus testing, more than a week after the health system began diverting patients from the emergency department to remote testing sites.
As workers directed cars to spots, patients, only a few with masks, rolled down their windows. Doctors and medical clinicians, in teams of two or three, headed out of the hospital into the rain with testing kits, collecting swabs and attending to patients.
As of Monday, Abington-Jefferson reported 47 positive patients, but no equipment shortages.
From the lobby of the hospital, Dr. Gerard Cleary, Abington’s chief medical officer, discussed the new safety protocol at the region’s hospitals, contingencies in place for added hospital space, sacrifices workers are making, and the challenges he anticipates in the upcoming weeks and months as the number of cases of those with COVID-19 is expected to rise.
“(The hospital) runs on all cylinders with all of our staff, nutritional support, environmental services, security. They are under the exact same pressures we are under, they are under the same risks we are under, and they worry about their families just as much as anyone else. Physicians and medical assistants who volunteered to be first on the line … they put themselves in immediate risk to do the right thing for the community.”
On the front lines @AbingtonJeff @TheIntellNews pic.twitter.com/QN37eMViVl
— Marion Callahan (@marioncallahan) March 24, 2020
‘I don’t know if I’ve come in contact with anyone or not’
“For me, I’m concerned about going in and out of my house every day, with my kids and wife around the house. I don’t know if I’ve come in contact with anyone or not.
“I heard that two cops came down with it yesterday. We are going into people’s houses interacting with them. Some people say they have it when they don’t. Some people don’t know. The 911 dispatch is doing a great job prescreening it, but they are talking to civilians who don’t have any medical training.”
Bucks County EMS worker
‘Don’t have the television or radio on 24/7’
“The social isolation is probably the thing I hear about the most. There is a big part of interpersonal communication that is visual. … When you’re forced to isolate at home or keep your distance from other folks, you need to find ways to make up for that deficit, using Skype, video conferencing, FaceTime on cellphones, just to reinforce that element that gets artificially taken out of most communication.
“… Don’t have the television or radio on 24/7. I would have a few trusted sources of information, like the CDC. Check those a couple of times of day, but certainly don’t immerse every waking moment listening to lots of information that may not turn out to be accurate. Keep up normal routines, when you go to sleep, when you get up … keep structure in your day. Make sure to schedule time for rest and relaxation. Go outside. Get physical exercise, which has great anti-anxiety, anti-depressant, anti-stress effects, and boost your immune system.
Dr. Diane Custer, chair of psychiatry, Abington-Jefferson Health
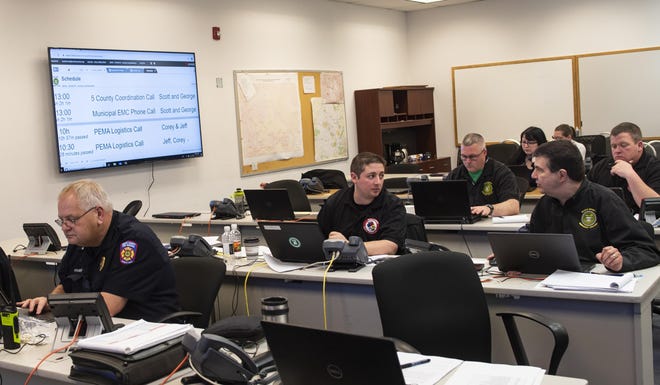
Protective supplies: ‘Our greatest request’
“… That’s probably our greatest request, personal protective equipment, not only from the public safety worker perspective but also from public health and our health care workers. The supply is not significant out there. … We have been working with many organizations and different companies and corporations to find resources.
“There are some things almost impossible to find.
“We are having a tough time finding surgical masks; we are having a tough time finding disposable surgical gowns, N95 masks. It is very difficult to find hand sanitizer and other cleaning supplies.
“… We’ve sent in resource requests to the state, Pennsylvania Emergency Management Agency, for different types of resources, in the way of masks, gowns and face shields, those types of things that would protect public safety and health care workers. … We are hoping they will be able to fulfill some of those because of the shortages.”
Scott Forster, director of Emergency Services, Bucks County
‘It kind of feels like Florida before the hurricane hits’
“… I have to say, there’s really not too much exciting going on at Doylestown, Grandview or Lansdale as of yet. The hospitals are not swamped with sick patients. Things are actually very quiet, because they’ve canceled everything elective. We are all waiting for a crisis which hasn’t occurred yet.
“It kind of feels like Florida before the hurricane hits. We were all waiting to see if it will make landfall.”
Central Bucks doctor, a specialist who works for three area hospital networks
Through this pandemic, we want to tell our readers and viewers about those on the front lines, bringing you their voices, struggles, suggestions and hopes. We need each other to stay connected, so please, keep your stories coming.